What is ICSI?
Intracytoplasmic sperm injection (ICSI) was developed in 1991 and the first baby conceived through ICSI was born the year after in 1992. ICSI was developed to assist fertilisation when sperm quality is particularly poor. Over the decades, ICSI has advanced into a more effective and reliable procedure. It is the preferred method for fertilisation in most ART centres around the world.
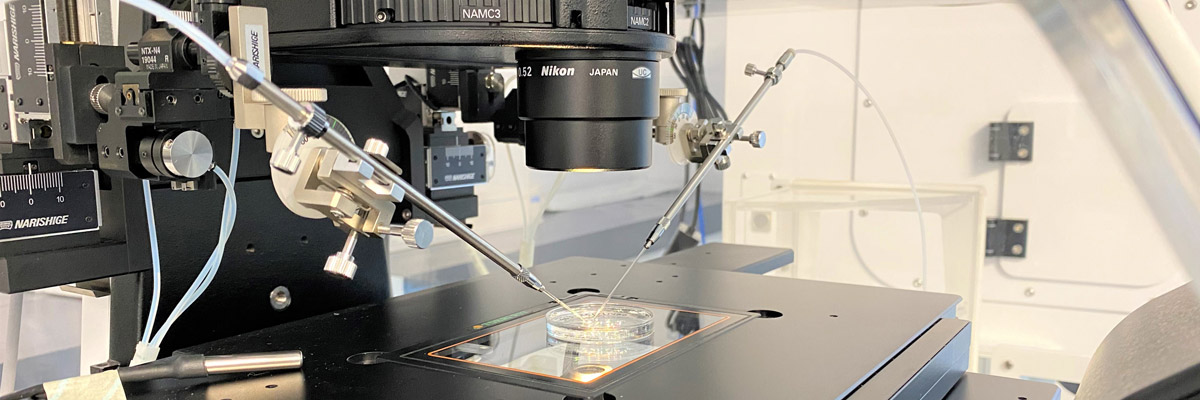
ICSI is a technique that involves the direct injection of a single sperm into an egg using a fine needle. ICSI is most useful for couples who suffer from severe male factor infertility as it bypasses the initial steps of gamete interaction.
As ICSI is a skill-based procedure, the expertise of the embryologist plays a significant role in ensuring good fertilisation. The entire process is done under microscopic visualization and micromanipulation using precision-based equipment. Healthy sperm is chosen and immobilised before being delivered into the egg’s cytoplasm.
When is ICSI used?
ICSI is often recommended if the patient:
- has poor sperm parameters (count, motility, morphology).
- has sperm that was surgically removed from the testicles or epididymis.
- has tried multiple cycles of IUI but was unsuccessful.
- has unexpectedly low fertilisation from previous IVF attempt.
What are the drawbacks of ICSI?
ICSI is a great tool to overcome issues with male factor infertility.
However, some of the disadvantages of ICSI are:
- damage to the eggs that may be incurred from the manipulation.
- overwriting the natural selection of “the-fittest” sperm that enters the egg.